- Research
- Open access
- Published:
Bacterial profile of surgical site infection and antimicrobial resistance patterns in Ethiopia: a multicentre prospective cross-sectional study
Annals of Clinical Microbiology and Antimicrobials volume 22, Article number: 96 (2023)
Abstract
Background
Globally, surgical site infections (SSI) are the most commonly reported healthcare-associated infections.
Methods
A multicentre study was conducted among patients who underwent surgical procedures at four hospitals located in Northern (Debre Tabor), Southern (Hawassa), Southwest (Jimma), and Central (Tikur Anbessa) parts of Ethiopia. A total of 752 patients clinically studied for surgical site infection were enrolled. The number of patients from Debre Tabor, Hawassa, Jimma, and Tikur Anbessa, hospitals was 172, 184, 193, and 203, respectively. At each study site, SSI discharge culture was performed from all patients, and positive cultures were characterized by colony characteristics, Gram stain, and conventional biochemical tests. Each bacterial species was confirmed using Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry (MALDI TOF). An antimicrobial susceptibility test (AST) was done on Mueller–Hinton agar using the disk diffusion method. Logistic regression analysis was used to assess associations of dependent and independent variables. A p-value < 0.05 was considered statistically significant. Data were analysed using STATA 16 software.
Results
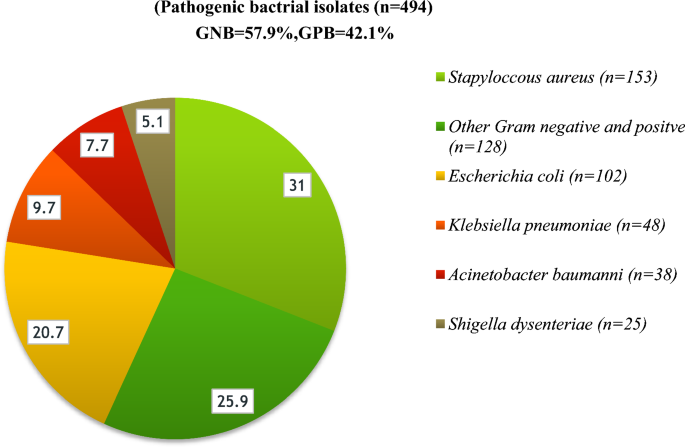
Among 752 wound discharge cultures performed, 65.5% yielded growth. Among these, 57.9% and 42.1% were Gram-negative and Gram-positive isolates, respectively. In this study, a total of 494 bacteria were isolated; Staphylococcus aureus (31%), Escherichia coli (20.7%), and Klebsiella pneumoniae (9.8%) were the most common. Rare isolates (0.8% each) included Raoultella ornithinolytica, Stenotrophomonas maltophilia, Alcalignes faecalis, Pantoea ecurina, Bacillus flexus, and Paenibacillus tylopili. Enterobacteriaceae showed high levels of resistance to most of the tested antibiotics but lower levels of ertapenem (32.9%), amikacin (24.3%), imipenem (20.3%), and meropenem (17.6%) resistance. Multidrug-resistant (MDR) frequency of Enterobacteriaceae at Debre Tabor, Hawassa, Jimma, and Tikur Anbessa hospitals was 84.5%, 96.5%, 97.3%, and 94%, respectively. Ages ≥ 61 years (AOR = 2.83, 95% CI: 1.02–7.99; P 0.046), prolonged duration of hospital stay (AOR = 4.15, 95% CI: 2.87–6.01; P 0.000), history of previous antibiotics use (AOR = 2.83, 95% CI: 1.06–2.80; P 0.028), history of smoking (AOR = 2.35, 95% CI: 1.44–3.83; P 0.001), emergency surgery (AOR = 2.65, 95% CI: 1.92–3.66; P 0.000), and duration of operation (AOR = 0.27, 95% CI: 0.181–0.392; P 0.000) were significant risk factors.
Conclusion
The most prevalent isolates from Gram-positive and Gram-negative bacteria across all hospitals were S. aureus and E. coli, respectively. Many newly emerging Gram-negative and Gram-positive bacteria were identified. Variation between hospitals was found for both SSI etiology type and MDR frequencies. Hence, to prevent the emergence and spread of MDR bacteria, standard bacteriological tests and their AST are indispensable for effective antimicrobial stewardship.
Introduction
Surgical site infection (SSI) is the major costliest healthcare-associated infection and a substantial cause of morbidity and mortality throughout the world [1, 2]. It occurs near or at the incision site and/or deeper underlying tissue spaces and organs within 30 days of a surgical procedure performed (or up to 90 days for implanted prosthetics) [3]. In low and middle-income countries SSI ranked the most frequently reported case of nosocomial infections [4], and in some settings, up to one-third of patients who are operated on [5] can catch SSI, despite standard protocols of preoperative preparation and antibiotic prophylaxis are practiced [6]. The SSI rate in Ethiopia has been reported to be between 14.8 and 20% [5, 7,8,9], and surgical patients account for 38% of general surgical wards at various teaching hospitals [10]. It results from mostly bacterial contamination during or after the surgical procedure but only a small portion progresses to clinical infection due to innate host defences removing contaminants. The contamination that will lead to surgical site infection depends on the dose of bacterial contamination, the virulence, and drug resistance of the bacteria [11]. Most SSI infections are preventable [11], however probable development of an infection depends on the age, immunocompromising conditions of the host, or the antimicrobial-resistance (AMR) nature of the infecting microorganisms [12]. The frequency varies from one hospital to the other and is related to complications [13]. Patients with SSI are twice as likely to die, 60% more likely to spend time in an intensive care unit (ICU), and more than five times more likely to be readmitted to the hospital after discharge [14]. The most common pathogens associated with surgical wound infections are Staphylococcus aureus, Escherichia coli, Klebsiella spp., Proteus spp., Citrobacter spp., Acinetobacter spp., Coagulase negative Staphylococcus aureus and pseudomonas aeruginosa [7, 15]. Beta-lactam antibiotics are the most widely used antibiotics for SSI prophylaxis and therapy; however, 30% to 90% of antibiotics are misused or overused [16, 17]. This inappropriate overuse increases selection pressure, favouring the emergence of drug-resistant bacteria, making the choice of empirical therapy more difficult and expensive, and poses a serious threat to public health, thus increasing the global risk of SSI [18, 19]. The condition is more serious due to irrational antimicrobial prescriptions and un-updated empirical therapy. Hence, the use of data from clinical laboratories' antibiotics susceptibility testing (AST) or solid epidemiological data from ongoing nosocomial infection surveillance is needed to minimize the problem [20]. In developing countries, including Ethiopia, published reports on bacterial pathogens and their antibiotics resistance patterns of frequently causing SSIs are relatively scarce [21] compared to the developed parts of the world. Besides, virtually all earlier reports depend on phenotypic laboratory methods to characterize pathogenic bacteria and studies were done at single sites with small sample sizes [9, 22, 23]. A recent systematic review and meta-analyses study by Birhanu Y et al. [24] focused on the pooled prevalence of SSI and its aetiology in Ethiopia. Also, the study had limitations, the papers included used only phenotypic laboratory methods and the result did not display AMR data. Thus, there have always been ambiguities in the interpretation of the findings when using phenotypic bacterial identification methods. In this study, to avoid the ambiguity in the interpretation of strain identification, we employed Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry (MALDI TOF) technique for the confirmation of bacterial isolates. Furthermore, this is comprehensive study with a large sample size conducted to determine the bacterial profile of surgical site infection and antimicrobial resistance patterns at four major hospitals in Ethiopia.
Methods
Study site and design
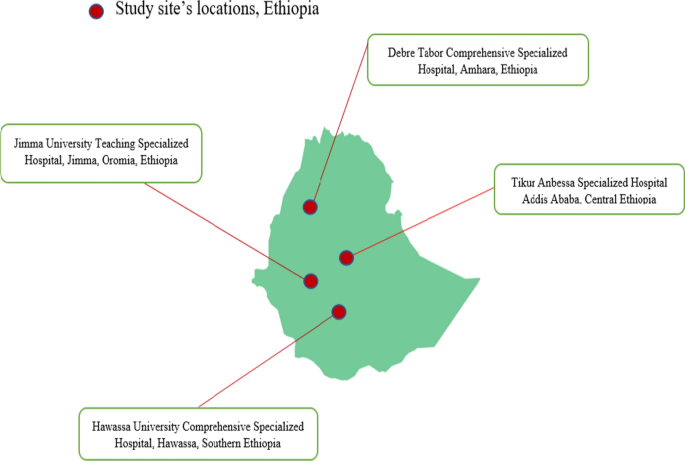
A multicentre cross-sectional study was conducted between July 2020 and August 2021 at four selected hospitals in Northern, Central, Southern and Southwest Ethiopia. The study was conducted in purposively selected University Teaching Hospitals in Ethiopia, namely, Debre Tabor Comprehensive Specialized Hospital (DTCSH), Hawassa University Teaching Hospital (HUTH), Jimma University Teaching Hospital (JUTH), and Tikur Anbessa Specialized Hospital (TASH) (Fig. 1).
DTCSH comprehensive specialized hospital provides health service to over 5 million people located in Debre Tabor town of South Gondar Administrative Zone, Amhara Regional State. Debre Tabor town is about 98 km away to the East of Bahir-Dar (the capital of Amhara regional state) and about 666 km North of Addis Ababa (the capital of Ethiopia). It is the only specialized hospital in the south Gondar Zone having over 400 beds.
The hospital provides surgery, pediatrics, emergency, maternity, gynecologic/obstetric, and psychiatric, including other departments. In addition, the hospital serves as a teaching centre for the region.
HUCSH is located in Hawassa city in Southern Ethiopia, 280 km from Addis Ababa. HUCSH is one of the largest health facilities in the Southern part of the country and provides teaching, public health services and research activities. It serves more than 20 million people locally and in the neighbouring regions. Currently, the hospital has over 400 beds and provides patient care to 90,200 outpatients, 18,100 hospitalized patients and 1100 emergency cases annually.
TASH is the teaching hospital of Addis Ababa University located in Addis Ababa, the capital of Ethiopia and the largest specialized hospital in Ethiopia, with over 700 beds. It is also an institution where specialized clinical services that are not available in other public or private institutions are rendered to the whole nation.
The TASH has 200 doctors, 379 nurses and 115 other health professionals dedicated to providing health care services. The various departments, faculties and residents under specialty training in the School of Medicine provide patient care in the hospital.
In their outpatient and inpatient units, the hospital offers a variety of services. They also have microbiology laboratories that perform culture and antimicrobial sensitivity testing.
While three hospitals had established microbiology laboratories the DTCSH had started performing bacteriological culture and antimicrobial susceptibility testing at the time of this study. Therefore, with the help of Armauer Hansen Research Institute (AHRI), DTCSH and my home institutions Debre Tabor University we established a bacteriology laboratory, which was used for wound culture processing and antimicrobial susceptibility testing.
Patient recruitment and sample size calculation
The source population the study participants drawn were all patients with suspected cases of SSI who were admitted for elective and emergency surgery. Those who developed signs and symptoms of SSI within 30 or 90 (received implant) days and gave consent and/or assent to participate in the study were enrolled and decision to identify eligible patients as SSI cases were done by attending physicians. All age groups were included, but patients who had been on antibiotic treatment within the preceding ten days, SSI later than 30 days after the operation, or refused to give assent or consent (participate in the study) as well as patients with infected burn wounds, were excluded from the study. A total of 752 clinically diagnosed cases of SSI from different wards were enrolled in the study. The sample size was calculated based on a single proportion sample size estimation formula (n = Z2 P (1—P) /d2) using a proportion of 20% [25]. As this was a multicenter study, to increasing the sample size a precision (d) of 0.03 was used, where Z stands for Z statistic with a level of confidence of 95%, and the Z value of 1.96. With a 10% non-response rate, the total sample size came to 752. A convenient sampling technique was used to recruit study participants until the required sample size was achieved, and proportional allocation was made among different hospitals based on the patient flow across the four study sites.
Operational definitions
Surgical site infection occurs near or at the incision site and/or deeper underlying tissue spaces and organs within 30 days of a surgical procedure performed (or up to 90 days for implanted prosthetics) [3].
Clean wound where no inflammation is encountered and the respiratory, alimentary or genitourinary tracts were not entered.
Clean contaminated wound is where the respiratory, alimentary or genitourinary tracts were entered but without significant spillage.
Contaminated when acute inflammation is encountered, or there is visible contamination of the wound.
Dirty wound wound in the presence of pus, where there is a previously perforated hollow viscous or compound/open injury more than four hours old [26].
Antibiotic a drug, which is products of fungi or bacteria that kills bacteria or inhibits their growth. Antibiotics are not effective against viruses (also referred to as an antimicrobial).
Multidrug resistance (MDR) refers to resistance at least one antimicrobial agent in three or more antimicrobial classes.
Data collection
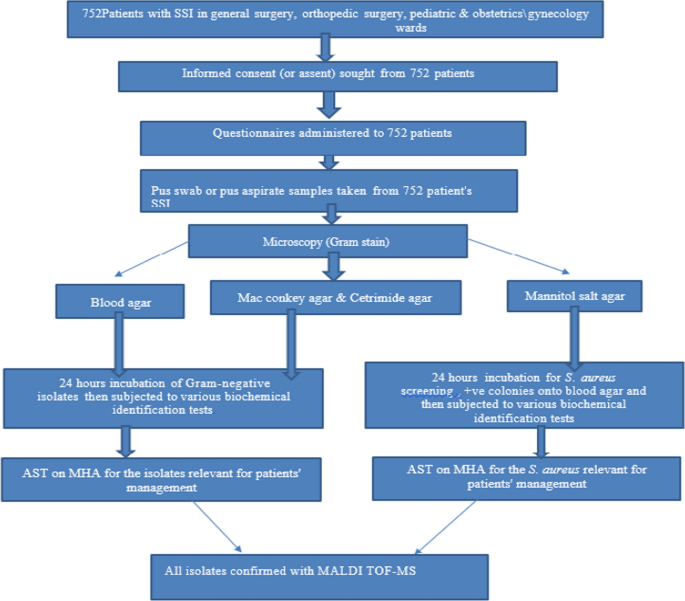
Professional nurses who had experience of wound swabs sample collection and microbiologists who were working in the bacteriology laboratory were recruited as data collectors. Training on socio-demographic and clinical data collection using structured questionnaires, wound swab sample collection and sample transportation to bacteriology laboratories and culture were given to all data collectors. Wound swab cultures, bacterial identification and drug susceptibility testing were performed in accordance with a standardized laboratory protocol that was uniformly applied in all study sites (Fig. 2). The findings of each culture were communicated to attending physicians for patient management. All bacterial strains were stored at − 80 °C and transported to the Armauer Hansen Research Institute (AHRI) and Sweden for further characterization. The isolates were transported to Sweden utilizing a triple packaging method with dry ice, specifically engineered for the safe carriage of Category A and B for Infectious and non-infectious substances, in accordance with UN regulation UN3373 for DNA samples and UN2814 for bacterial isolates.
Sample collection and transportation
Trained personnel collected SSI discharge aseptically (pus, pus aspirates, and wound swabs) with sterile syringe with needle pus aspirate or sterile cotton-tipped swabs from inside to outside. After cleaning the infected area with 10% povidone-iodine, a sterile cotton-tipped swab was placed in the center, and the rolling technique was used. All wound swabs were dipped in modified Stuart's Transport Medium and immediately transported to the bacteriology laboratory for culture and drug susceptibility testing within 1 h. Following that, all collected specimens were processed for the identification of bacteria implicated in SSIs.
Biochemical tests
For the final identification of the isolates, the following biochemical tests were performed using colonies from pure cultures. For Gram-negative rods, gas production, sugar fermentation, H2S production, indole production, citrate utilization, lysine decarboxylase production, urea hydrolysis, and motility tests were used. Gram-positive cocci were identified using the results of the Gram reaction, catalase, coagulase, bacitracin, and optochin tests [27].
Bacterial strain confirmation using matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS)
The isolates were transported to Sweden utilizing a triple packaging method with dry ice, specifically engineered for the safe carriage of Category A and B Infectious and non-infectious substances. All bacteria were re-identified and confirmed using MALDI-TOF MS at the Clinical Microbiology Department of Uppsala University Hospital Uppsala, Sweden. From fresh cultures, a single colony of bacteria was smeared onto a MALDI-TOF plate, and the sample was air-dried. Next, 1 µl of formic acid was added to each cell and air-dried, and then 1 µl of MALDI matrix solution was applied to the cells and air-dried before reading. MALDI-TOF identification was automatically scored by the system software between 1 and 3 points. All isolates with scores two and above were accepted, and all results below 1.7 and flagged red were rejected. Samples with scores 1.7–2 and flagged yellow were re-analysed.
Antimicrobial susceptibility testing (AST)
The antibiotics susceptibility tests were performed on Muller-Hinton agar (Oxoid) by using the Kirby-Bauer disk diffusion technique. Using a sterile wire loop, 3–5 pure colonies were transferred to a tube containing 5 mL of sterile normal saline (0.85% NaCl) and gently mixed until a uniform suspension formed. Standard inoculum density was adjusted to 0.5 McFarland units. The excess broth suspension was removed by tapping against the tube wall. The bacterial suspension was swabbed on MHA surface by using sterile swab then a set of antibiotic discs placed with sterile forceps at least 24 mm apart from one another [28]. All antibiotics discs were OXOID products (Oxoid Ltd, UK), and susceptibility of Gram-negative isolates was tested against: ampicillin (10 µg), gentamicin (10 µg), amikacin (30 µg), ciprofloxacin (5 µg), chloramphenicol (30 µg), ceftazidime (30 µg), cefotaxime (30 µg), ceftriaxone (30 μg), cefuroxime (30 µg), cefepime (30 µg), tetracycline (30 µg), amoxycillin + Clavulanate (20/10 μg), Trimethoprim-sulfamethoxazole (1.25/23.75 µg), ampicillin-sulbactam (10/10 µg), aztreonam (30 µg), meropenem (10 µg), Imipenem (10 µg), ertapenem (30 µg). Gram-positive isolates were tested against penicillin (10units), ampicillin (10 µg), vancomycin (30 µg), erythromycin (15 µg), ciprofloxacin (5 µg), cefoxitin (30 µg), clindamycin (30 µg), erythromycin (15 µg), doxycycline (30 µg), chloramphenicol (30 µg), gentamicin (10 µg), and oxacillin (5 µg), tetracycline (30 µg), [28]. Following that, the plates were incubated at 37 °C for 18–24 h. Each zone of inhibition was measured to the nearest millimeter, and classified as sensitive, intermediate, or resistant using the standard technique [28]. MDR was a bacterium that was simultaneously resistant at least one drug in three or more categories.
Quality control
All specimens were collected according to the standard operating procedure (SOP) [21]. A double data entry method was used to ensure the accuracy of the data. The performance of all prepared media was checked by inoculating control strains, E. coli (ATCC 25922) and S. aureus (ATCC 25923), for each new batch of agar plates [22]. In addition, the sterility of culture media was checked by incubating 5% of the prepared media at 37 °C for 24–48 h. In addition, reagents for Gram-stain and biochemical tests were checked against control strains of S. aureus and E. coli. The 0.5 McFarland standard was used to standardize the inoculum density of the bacterial suspension for the susceptibility test. Each MALDI-TOF run also included quality control strains using E. coli (ATCC 25922) and S. aureus (ATCC 25923).
Data analysis
The data were checked for completeness, missing values, and coding of questionnaires entered into Research Electronic Data Capture (RED-Cap) and exported to STATA version 16.0. Frequencies and cross-tabulations were used to summarize descriptive statistics (median, percentages or frequency). Associations of possible risk factors with SSIs was assessed using bivariate and multivariate logistic regression to study the effect of independent variables on the dependent variables. P-value less than 0.05 were considered statistically significant.
Ethical considerations
The Department of Medical Microbiology, Immunology, and Parasitology (DMIP) and the AHRI/ALERT Research Ethics Committee (AAREC) reviewed and approved the study, and institutional review board (IRB) approval was obtained from Addis Ababa University's College of Health Sciences and AAREC, AAUMF03-008/2020. Written permission letter was obtained from each study site before starting the data collection. The purpose and procedures of the study was explained to the study participants, participants’ parents or guardians before recruitment to the study. Those study participants who gave written informed consent and those children whose parents or guardians gave informed assent were selected and enrolled in this study. Results obtained from all patients were communicated to attending physicians and all patient’s information was kept confidentially.
Results
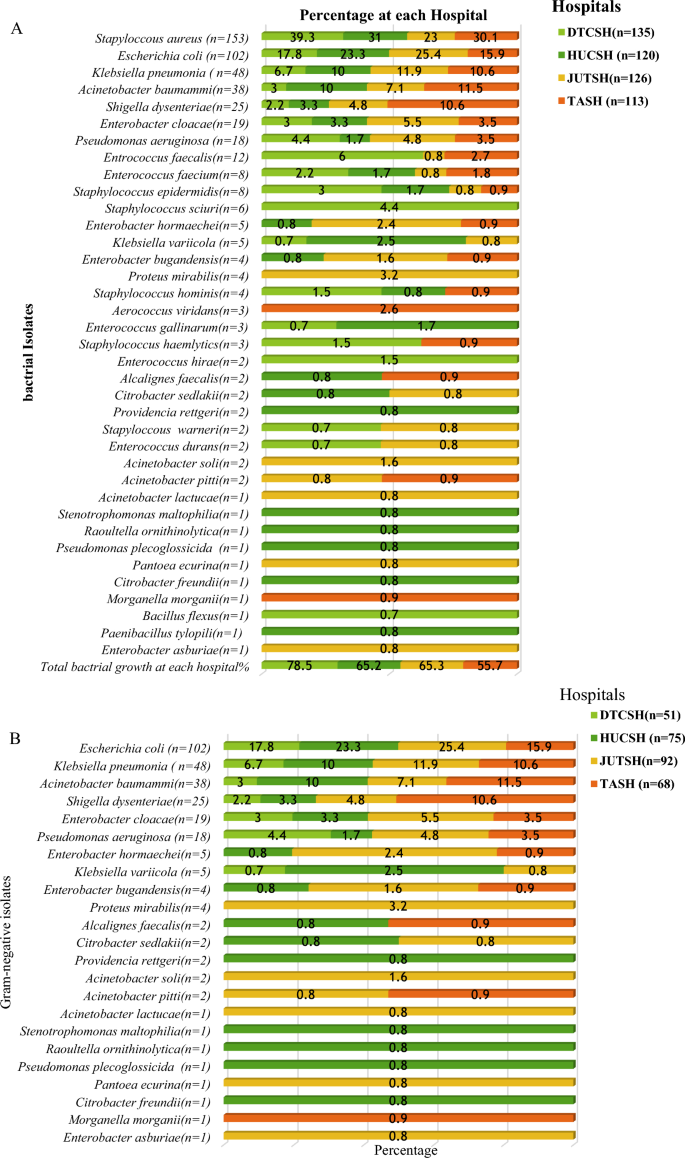
In the present study, a total of 752 patients from four different hospitals were investigated for SSIs. The number of patients from DTCSH was172, and the numbers from HUCSH, JUSTH, and TASH, were184, 193, and 203, respectively (Table 1). Of the 752 study participants whose SSI discharge was inoculated onto growth media, 65.5% (493 /752) showed bacterial growth (Table 1). DTCSH had the highest percentage of positive cultures (78.5%), followed by JUTSH (65.3%), and HUCSH and TASH, respectively, had 65.2% and 55.7% of SSI bacterial growth (Table 1). The study participants age ranged from 3 days to 85 years with median of 28 years and 418 (55.6%) were males. Approximately 487 (64.8%) of patients had deep SSI, 454 (60.4%) preoperative hospital stay > 7 days, 619 (82.4%) history of hospital admission, 388 (52.9%) had previous use of antibiotics, 448 (59.6%) had smoking history, 506 (67.2%) of surgical procedures were emergency surgery, 724 (96.2%) of patients with clean or clean contaminated wounds dominated the wound class, 548 (72.8%) required antimicrobial prophylaxis before the procedure, and 55.3% underwent surgeries lasting greater than an hour (Table 1).
Bivariate and multivariable logistic regression analyses were used to see the relationship between the independent variables over the dependent variable. On bivariate regression analysis, male sex, age ≥ 61, SSI type, preoperative hospital stays, history of hospital admission, previous use of antibiotics, smoking, emergency surgery, and duration of operation ≥ 1 h had a statistically significant association with the occurrence of SSI. The type of surgery (wound), alcohol history and the timing of prophylactic antibiotics ≥ 1 h had no statistically significant association (Table 2). The result of the multivariate regression showed that ages ≥ 61 years (AOR = 2.83, 95% CI: 1.02–7.99; P 0.046), prolonged duration of hospital stay (AOR = 4.15, 95% CI: 2.87–6.01; P 0.000), history of previous antibiotics use (AOR = 2.83, 95% CI: 1.06–2.80; P 0.028), history of smoking (AOR = 2.35, 95% CI:1.44–3.83; P 0.001), emergency surgery (AOR = 3.24, 95% CI: 2.29–4.77; P 0.000), and duration of operation (AOR = 0.27, 95% CI: 0.181–0.39; P 0.000) were significant risk factors (Table 2).
Frequency and distribution of identified bacterial isolates
The total number of pathogenic bacterial isolates were 65.7% (494/752) from all SSI culture (Figs. 3, 4A). Gram-negative were 57.9% (286/752), and Gram positive 42.1% (208/752) according to Fig. 2B, C). Of these, 2.6% (13/493) of cultures were a mixture of two colony types, while 2.4% (12/493) were commensals or contaminants and 97.4% showed single bacterial growth. Species of the mixed cultures were Raoultella ornithinolytica, Paenibacillus tylopili, S. aureus and coagulase negative staphylococci. Among the identified types of bacteria, Staphylococcus aureus was the predominant one (31%), followed by E. coli (20.7%) and Klebsiella pneumonia (9.8%) among SSIs (Fig. 1). Other less frequently detected species were Acinetobacter baumannii (7.6%), Enterobacter cloacae (5.1%), Pseudomonas aeruginosa (3.7%), Klebsiella variicola, and Enterobacter hormaeche (1% each). Diverse species of Acinetobacter, Enterobacter, Enterococcus, Staphylococcus, Aerococcus, Bacillus, Citrobacter, and Pseudomonas were identified. While Gram-positives was found at all four hospitals (42.1%), it was mainly detected at DTCSH (40.4%), with 21.6%, 21.6%, and 16.3% isolated at TASH, HUCSH, and JUTSH, respectively (Fig. 2B). In addition, Raoultella ornithinolytica, Stenotrophomonas maltophilia, Pantoea ecurina, Providencia rettgeri, Alcalignes faecalis, and Morganella morganii were detected as rare bacterial pathogens. Figure 2A shows the frequency and distribution of Gram-negative bacterial isolates at the four hospitals.
Frequency and distribution of bacteria isolated from patients investigated for surgical site infection at four different hospitals in Ethiopia. GNB Gram-negative bacteria, GPB Gram-positive bacteria, Other GN and GP (n = 128): Raoultella ornithinolytica (n = 1), Stenotrophomonas maltophilia (n = 1), Acinetobacter soli (n = 2), Acinetobacter pitti (n = 2), Acinetobacter lactucae (n = 1), Pseudomonas plecoglossicida (n = 1), Pantoea ecurina (n = 1), Citrobacter freundii (n = 1), Citrobacter sedlakii (n = 2), Providencia rettgeri (n = 2), Alcalignes faecalis (n = 2), Proteus mirabilis (n = 4), Morganella morganii (n = 1), Aerococcus viridans (n = 3), Bacillus flexus(n = 1) Paenibacillus tylopili (n = 1), Enterobacter cloacae (n = 19), Enterobacter asburiae (n = 1), Enterobacter bugandensis (n = 4), Enterobacter hormaeche (n = 5), Enterococcus faecium (n = 8): Enterococcus gallinarum (n = 3), Enterococcus hirae (n = 2), Enterococcus durans (n = 2), Staphylococcus hominis (n = 4), Staphylococcus haemolyticus (n = 3), Staphylococcus warneri (n = 2), Staphylococcus sciuri (n = 6), S. epidermidis (n = 8)
Frequency and distribution of bacterial isolates from the total number of bacteria isolated at each hospital A total identified bacteria at each site, B Gram-negative isolates and C Gram-positive isolates. DTCSH Debre Tabor Comprehensive Specialized Hospital, HUCSH Hawassa University Comprehensive Specialized Hospital, JUTSH Jimma University Teaching Specialized Hospital, TASH Tikur Anbessa Specialized Hospital, n number of bacterial isolates
Antibiotic resistance pattern of SSI bacterial isolates
The predominant isolate from Gram-positives, S. aureus, revealed a high level of resistance toward penicillin 90.1%, and ampicillin 76.5%, while 7.8%, 10.6%, and 12.4% of the isolates were resistant to clindamycin, chloramphenicol, and gentamicin respectively but 100% of S. aureus were sensitive to vancomycin (Table 3). All isolates of S. aureus showed multiple drug resistance (resistance to two or more drugs).
Cefoxitin, which is a surrogate marker of methicillin, showed 22.7% resistance against S. aureus. Enterococcus species showed 70.4% resistance to ampicillin and 66.7% to erythromycin. Table 3 shows the AMR pattern of Gram-positive bacteria.
The Enterobacteriaceae showed high resistance toward ampicillin (93.2%), ceftriaxone (90.5%), cefuroxime (88.7%), aztreonam (82.9%), ceftazidime (80.6%), cefepime (77%), ampicillin-sulbactam (76.1%), trimethoprim-sulfamethoxazole (77.5%), tetracycline (72.5%), amoxicillin-clavulanic acid (71.2%) (Table 4).
Low resistance frequency of Enterobacteriaceae was detected for amikacin (24.3%), imipenem (20.3%), meropenem (17.6%), and ertapenem (32.9%) (Table 4).
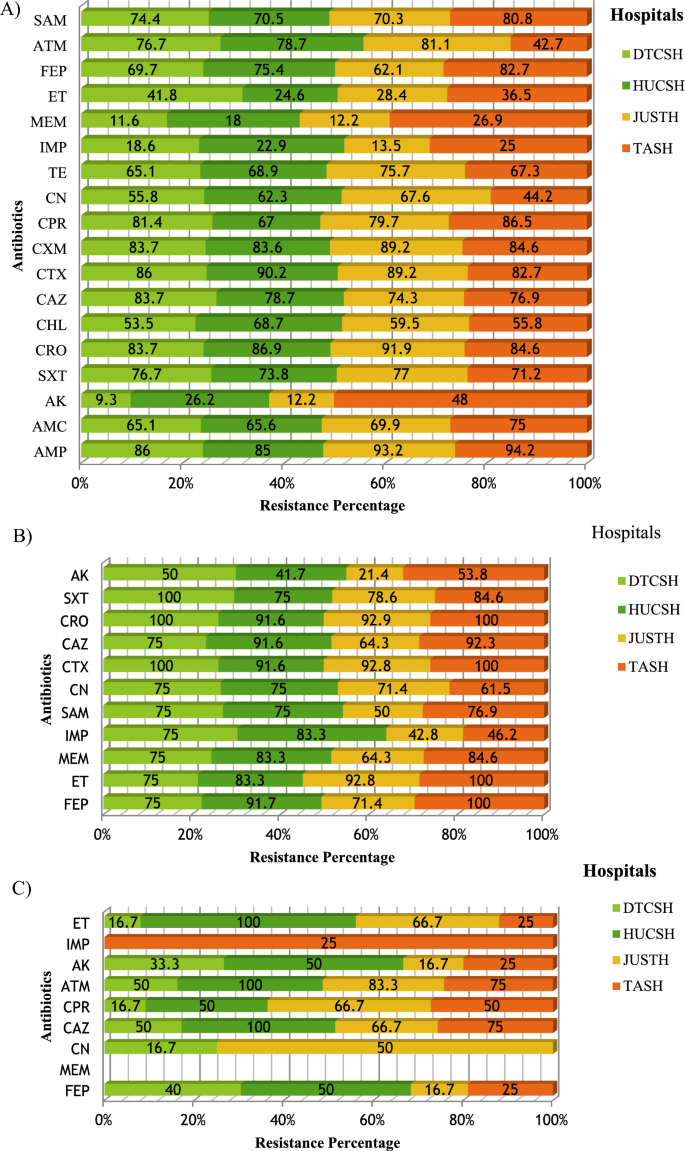
The resistance of Enterobacteriaceae to meropenem and imipenem was (11.6%,18.6%), (18%, 22.9%), (12.2%,13.5%) and (26.9%,25%) at DTCSH, HUCSH, JUTSH, and TASH, respectively (Fig. 5A).
Frequency of antibiotic resistance at four hospitals; A Enterobacteriaceae B Acinetobacter species C Pseudomonas species. The percentage represents the numbers of resistant isolates, out of the total number of isolates at all hospitals. AMP ampicillin, AMC amoxicillin/clavulanate, AK amikacin, SXT trimethoprim-sulfamethoxazole, C chloramphenicol, CAZ ceftazidime, CTX cefotaxime, CRO ceftriaxone, CXM cefuroxime, CIP ciprofloxacin, CN gentamicin, TE tetracycline, ATM aztreonam, SAM ampicillin-sulbactam, FEP cefepime, IMP Impemene, MEM meropeneme, ET Ertapeneme, DTCSH Debre Tabor Comprehensive Specialized Hospital, HUCSH Hawassa University Comprehensive Specialized Hospital, JUTSH Jimma University Teaching Specialized Hospital, TASH Tikur Anbessa Specialized Hospital
The predominant isolate, E. coli (n = 102) revealed a high level of resistance to ampicillin (94.6%), ceftriaxone (99%), cefotaxime (93.8), ceftazidime (79.4%), cefepime (77%), cefuroxime (73.5%), ampicillin-sulbactam (72%), trimethoprim-sulfamethoxazole (71.5%), tetracycline (70.6%), and low-level resistance to gentamicin (57.8%), chloramphenicol (41.2%), ertapenem (24.5), imipenem (11.6%), amikacin (10.8%), meropenem (9.8).
K. pneumoniae (n = 48) were resistant to ampicillin (100%), ceftriaxone (100%), cefotaxime (93.8%), amoxicillin-clavulanic acid (91.7%), ceftazidime (88.5%), cefepime (81.2%), cefuroxime (77.1%), tetracycline (66.7%), ertapenem (43.8%), meropenem (41.7%), amikacin (33.3%), imipenem (29.2%). Amikacin and meropenem were 100% effective against all of the isolates of Klebsiella variicola and Proteus mirabilis. In the non-fermenter group, A. baumannii showed the highest resistance to cefotaxime (95.3%), ertapenem (92.1%), ceftazidime (89.5%), gentamicin (86.8%), cefepime (84.2%), meropenem (84.2%), and SXT (81.4%). In addition, A. baumannii has lower-level resistance to imipenem (65.9%) and ampicillin-sulbactam (63.1%) (Table 4). The resistance frequency of Acinetobacter species to meropenem at DRH, HUCSH, JUSTH, and TASH was 75%, 83.3%, 42.8%, and 46.2%, respectively (Fig. 3B). P. aeruginosa showed minimal resistance to ceftazidime (66.7%), cefepime (55.5%), gentamicin (47.8%), ciprofloxacin (22.2%), and amikacin (10.5%) (Table 4). In addition, 100% and 94.5% of Pseudomonas species were sensitive to meropenem and imipenem, respectively (Table 4, Fig. 5C).
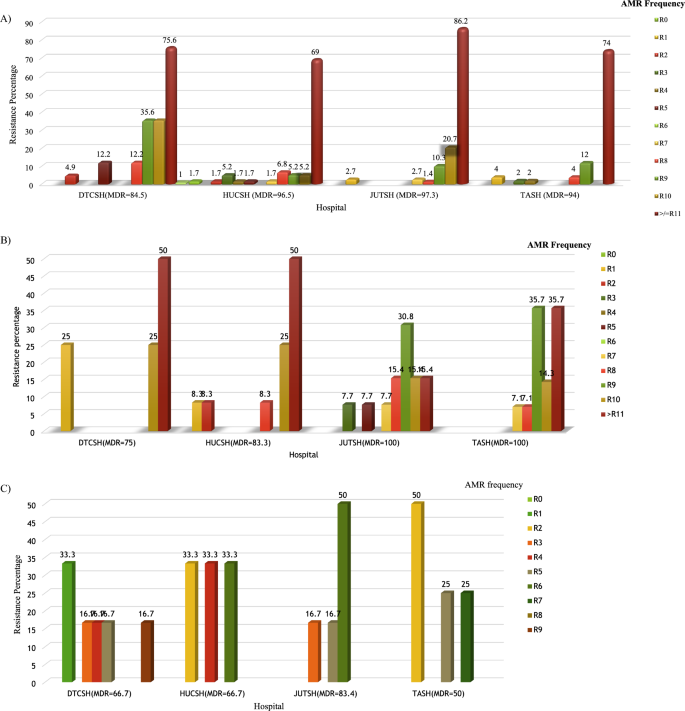
Multidrug resistance
The overall Multidrug resistance (MDR) to three or more antibiotics was observed in 100% of S. aureus (Table 3) and 93.3% Enterobacteriaceae (Table 4). Enterobacteriaceae that showed MDR to eight (R-9), nine (R-10) and ten (R- ≥ 11) antibiotics from different groups had a frequency of 6.3%, 6.7%, and 64.9%, respectively. Only 0.5% Enterobacteriaceae showed zero resistance (R-0) to all antibiotic classes tested, whereas 3.1% Enterobacteriaceae showed resistance to one antibiotic (R-1) class. For Enterobacteriaceae, the MDR frequency at DTCSH, HUCSH, JUSTH, and TASH was 84.5%, 96.5%, 97.3%, and 94%, respectively (Fig. 6A). E. coli, K. pneumoniae, E. cloacae, S. dysenteriae, K. variicola, and P. mirabilis showed an overall MDR frequency of 96.1%, 95.9%, 79.3%, 82%, 100%, and 100%, respectively. The overall MDR frequency of A. baumannii and P. aeruginosa was 95% and 77.8%, respectively. The MDR frequency for Acinetobacter species was 73% at DTCSH, 83.3% at HUCSH, 100% at JUTSH, and 100% at TASH (Fig. 4B). On the other hand, MDR frequency for Pseudomonas species was 66.7%, 66.7%, 83.3% and 50% at DTCSH, HUCSH, and JUSTH and TASH, respectively (Fig. 6C).
Frequency of multidrug resistance at four hospitals. A Enterobacteriaceae B Acinetobacter species C Pseudomonas species. Percentages represent the number of resistant isolates out of the total number of isolates at each hospital. Debre Tabor Comprehensive Specialized Hospital (DTCSH), HUCSH Hawassa University Comprehensive Specialized Hospital, and Jimma University Teaching Specialized Hospital (JUTH) and Tikur Anbessa Specialized Hospital (TASH), MDR multidrug resistance
Discussion
In surgically treated patients, post-operative SSI is still one of the leading causes of morbidity and mortality, and it increases the cost of health care due to repeated readmission. In order to effectively manage bacterial infection, it is crucial to identify the bacterial pathogens and choose an antibiotic that is efficient against the organism [1, 2].
As far as risk factors associated with the occurrence of SSI are concerned, in the present study, the likelihood of SSI occurrences among patients aged ≥ 61 years increased by a factor of 2.8. Similar findings have been conducted in Ethiopia [15, 16, 29] and elsewhere [30]. This might be due to a weakened immune response to infectious agents and poor nutritional status [31].
Patients who had a longer duration of hospital stay developed SSIs 4.1 times more frequently (P = 0.000) than those who had shorter time. This finding was in agreement with many studies in Ethiopia [29, 32, 33] and elsewhere [30]. This is a notable finding because it is associated with additional costs in a country with a staggering economy and healthcare system [34].
Similarly, the present study demonstrated that with previous use of antibiotics, patients had a 2.8 times higher chance of developing SSI than with non-previous use of antibiotics [35]. This could be because broad-spectrum antibiotics have a high risk of causing superinfection of resistant strains due to selective pressure [18, 19].
The type of surgery was also statistically associated with SSI in the present study. Undergoing emergency surgery showed approximately 3.24 times higher chances of acquiring SSIs when compared to elective surgery (P = 0.000), which complies with related studies [35].
The risk of developing SSI with smoking histories was found to be 2.35 times more than in those who did not have smoking history. There was a significant association between smoking patients’ history and SSI (P = 0.001). This finding was in agreement with smoking history were independent predictors of SSIs in multivariate logistic regression analysis [36]. Smoking weakens immunity and increases the risk of SSI [37].
The overall culture positivity rate from patients with SSI in the current study was 65.5%. Similar results reported from India (68%) [38]. Which was slightly smaller than results previously reported from Jimma (71.7%) [9]. In contrast, the current study was lower than reports from Tikur Anbessa (75.6%) [39], Gondar (83.9%) [40], and elsewhere (82%) [41]. Lower rates of positive culture were reported from India Bangladesh (61.8%) [42].
In this study, the Gram-negative bacterial isolation rate was greater (57.9%) than the Gram-positive isolates (42.1%), which is comparable with the study done in Addis Ababa [43]. On the other hand, the current study was lower in Gram- negative isolates than reports from Mizan-Tepi (73.2%) and higher in Gram-positive isolates (24.8%) [22]. This could be due to a difference in the study population.
In the current study, the profiles of bacterial isolates highly associated with SSI were S. aureus (31%), followed by E. coli (20.7%), and K. pneumoniae (8.9%). Studies from Gondar [44], Addis Ababa [45], and India [40] reported similar results. The high prevalence of S. aureus infection could be due to an endogenous source as well as environmental contamination.
In contrast to previous reports, a study from Addis Ababa found E. coli 23.1%, followed by multidrug-resistant Acinetobacter species 22.1% [34]. Similarly, in a study done by Jimma, E. coli was frequently identified and followed by Klebsiella spp. [41]. This variation in the distribution pattern of bacterial isolates may be due to the diversity of the study population, setting, and local antimicrobial usage pattern, which leads to the introduction of pathogens that may be resistant to currently used antibiotics.
Rare surgical site infections isolate including Raoultella ornithinolytica, Stenotrophomonas maltophilia, Alcalignes faecalis, and Paenibacillus tylopili, were identified. Such newly emerging bacteria-causing infections in SSI patients may result in future challenges [46,47,48]. These species, along with K. variicola and Pantoea ecurina, have never before been identified in patients in Ethiopia who were being evaluated for SSI. The isolation of these new SSI etiologies emphasizes the necessity of institution-based diagnostic and intervention practices.
In our finding, S. aureus revealed a high level of resistance to penicillin (88.6%) and ampicillin (77.3%), which was comparable to study in Turkey [46]. On the other hand, all isolated S. aureus were susceptible to vancomycin, and our finding was the same as earlier studies in Jimma [36] and Turkey [46].
Gram-negative bacteria showed higher resistance to ampicillin (93.2%), ceftriaxone (90.5%), cefuroxime (88.7%), aztreonam (82.9%), ceftazidime (80.6%), cefepime (77%), ampicillin-sulbactam (76.1%), trimethoprim-sulfamethoxazole (77.5%), tetracycline (72.5%), and amoxicillin-clavulanic acid (71.2%). Since β-lactam antibiotics are the most widely used antibiotics, many studies in Ethiopia [11, 34] and around the world have found similar resistant patterns [40]. This shows antibiotics require a periodic evaluation and the establishment of antibiotic policies for prophylaxis and treatment guidelines in the Ethiopian setting.
In this study, multidrug resistance (MDR) was observed (100%) in S. aureus and (93.4%) in Gram-negative bacteria, similar to findings from Bahir Dar [18].
In the current study, A. baumannii showed the highest to resistance cefotaxime (95.3%), ceftazidime (89.5%), gentamicin (86.8%), cefepime (84.2%), and trimethoprim-sulfamethoxazole (81.4%). Many studies have found that these organisms have a high resistance to the most commonly used antibiotics [34, 47, 48]. In addition, A. baumannii also showed remarkably high resistance to ertapenem (92.1%), meropenem (84.2%), and imipenem (65.9%).
Amikacin and meropenem were 100% effective against all of the isolates of P. mirabilis and K. variicola in our study. However, studies done in Mekelle [37], and elsewhere [29] showed that ciprofloxacin were effective against Proteus and Pseudomonas isolates. The differences maybe the rational use of antibiotics and the fact that the cost of the drugs may be higher relative to others, so people do not take these drugs for self-medication in the study area [49].
Carbapenem resistance among Enterobacteriaceae was 17.6%, 20.3%, and 32.9% to meropenem, imipenem, and ertapenem, respectively. Effective treatment options for Enterobacteriaceae were limited to amikacin, meropenem, and imipenem. The most frequent isolate is E. coli, which showed the highest resistance to ampicillin (ceftriaxone, cefotaxime, ceftazidime, cefepime, cefuroxime, ampicillin-sulbactam, trimethoprim-sulfamethoxazole, and tetracycline. Similar studies were conducted in Ethiopia [33] and Iraq [50]. This might be due to the indiscriminate use of antibiotics in both hospitals [18, 19].
In our study, an alarming level of carbapenem-resistant E. coli to ertapenem (24.5%), imipenem (11.8%), and meropenem (9.8%) was detected; however, it was lower than in another study [51]. The cause of the higher rates compared to other settings may be irrational use or misuses of antibiotics. The discrepancy of antibiotics resistance across sites includes differences in the rational use of antibiotics [52].
Strengths and limitation
The strength of this study was multicentred, enrollment of all age groups, a reasonably large sample size and re-characterizing bacteria using MALDI TOF–MS an advanced bacterial identification method, and the limitation were unable to investigate anaerobic bacterial and fungal agents due to limited laboratory resources at the hospitals.
Conclusions
This multicenter study identified frequent and diverse Gram-negative and Gram-positive SSI etiologies without significant variation in primary etiologies between hospitals. Isolation of various newly emerging bacterial strains in all sites showed the growing epidemiology and diversity of SSI etiologies. E. coli and S. aureus were the leading Gram-negative and Gram-positive isolates, respectively. High antimicrobial resistance was detected with varying frequency between hospitals. Gram-positive isolates revealed maximum sensitivity to vancomycin and clindamycin, whereas, among Gram-negative isolates, amikacin, imipenem, and meropenem were the most effective antibiotics Furthermore, the overall ceftriaxone resistance is about 90.5%. Among the study participants, 72.1% took prophylaxis and developed SSIs. The finding of high levels of carbapenem resistance, especially towards ertapenem, is alarming.
Hence, to prevent the emergence and spread of MDR SSI, we recommend effective antimicrobial stewardship and antibiotic treatment to based on AST of the pathogens. At the national level, regular surveillance and monitoring of antimicrobial resistance patterns are indispensable. This includes the careful monitoring of the antibiotics used as prophylaxis and empiric treatment by the concerned authorities.
Availability of data and materials
The data sets generated during and/or analysed during the current study are available from the corresponding authors on reasonable request.
Abbreviations
- AAERC:
-
AHRI/ALERT Ethics Review Committee
- AHRI:
-
Armauer Hansen Research Institute
- AMR:
-
Antimicrobial resistance
- AST:
-
Antimicrobial susceptibility testing
- ATCC:
-
American Type of Culture Collection
- CDC:
-
Center for Disease Control and Prevention
- CLSI:
-
Clinical Laboratory Standards Institute
- DMIP:
-
Department of Microbiology Immunology and Parasitology
- DTTRH:
-
Debre Tabor Teaching, and Referral Hospital
- HUTH:
-
Hawassa University Teaching Hospital
- JUTH:
-
Jimma University Teaching Hospital
- MALDI-TOF MS:
-
Matrix-assisted laser desorption ionization-time of flight mass spectrometry
- MDR:
-
Multi drug resistance
- MHA:
-
Mueller Hinton Agar
- SOP:
-
Standard operation procedure
- SSI:
-
Surgical site infections
- STATA:
-
South Texas Art Therapy Association
- TASH:
-
Tikur Anbessa Specialized Hospital
- ESBL:
-
Extended-spectrum beta lactamases
References
Forrester JD, Maggio PM, Tennakoon L. Cost of health care-associated infections in the United States. J Patient Saf. 2022;18(2):e477–9.
Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017;152(8):784–91.
Borchardt RA, Tzizik D. Update on surgical site infections: the new CDC guidelines. Jaapa. 2018;31(4):52–4.
Lewis SS, Moehring RW, Chen LF, Sexton DJ, Anderson DJ. Assessing the relative burden of hospital-acquired infections in a network of community hospitals. Infect Control Hosp Epidemiol. 2013;34(11):1229–30.
Mengesha RE, Kasa BG-S, Saravanan M, Berhe DF, Wasihun AG. Aerobic bacteria in post surgical wound infections and pattern of their antimicrobial susceptibility in Ayder Teaching and Referral Hospital, Mekelle, Ethiopia. BMC Res Notes. 2014;7(1):575.
Raza MS, Chander A, Ranabhat A. Antimicrobial susceptibility patterns of the bacterial isolates in post-operative wound infections in a tertiary care hospital, Kathmandu, Nepal. Open J Med Microbiol. 2013;3(3):159.
Godebo G, Kibru G, Tassew H. Multidrug-resistant bacterial isolates in infected wounds at Jimma University Specialized Hospital, Ethiopia. Ann Clin Microbiol Antimicrob. 2013;12:17.
Halawi E, Assefa T, Hussen S. Pattern of antibiotics use, incidence and predictors of surgical site infections in a Tertiary Care Teaching Hospital. BMC Res Notes. 2018;11(1):538.
Misha G, Chelkeba L, Melaku T. Bacterial profile and antimicrobial susceptibility patterns of isolates among patients diagnosed with surgical site infection at a tertiary teaching hospital in Ethiopia: a prospective cohort study. Ann Clin Microbiol Antimicrob. 2021;20(1):33.
Spagnolo A, Ottria G, Amicizia D, Perdelli F, Cristina ML. Operating theatre quality and prevention of surgical site infections. J Prev Med Hyg. 2013;54(3):131.
National Institute for Health and Care Excellence: Clinical Guidelines. Surgical site infections: prevention and treatment. London: National Institute for Health and Care Excellence (NICE). Copyright © NICE 2020. 2020.
Moradali MF, Ghods S, Rehm BHA. Pseudomonas aeruginosa lifestyle: a paradigm for adaptation, survival, and persistence. Front Cell Infect Microbiol. 2017;7:39.
Isibor JO, Oseni A, Eyaufe A, Turay A. Incidence of aerobic bacteria and Candida albicans in post-operative wound infections. Afr J Microbiol Res. 2008;2(11):288–91.
Organization WH. Global guidelines for the prevention of surgical site infection. Geneva: WHO; 2016.
Biadglegne F, Abera B, Alem A, Anagaw B. Bacterial isolates from wound infection and their antimicrobial susceptibility pattern in Felege Hiwot referral Hospital North West Ethiopia. Ethiop J Health Sci. 2009;19(3).
Mulu W, Kibru G, Beyene G, Damtie M. Postoperative nosocomial infections and antimicrobial resistance pattern of bacteria isolates among patients admitted at Felege Hiwot Referral Hospital, Bahirdar, Ethiopia. Ethiop J Health Sci. 2012;22(1):7–18.
Munckhof W. Antibiotics for surgical prophylaxis. Aust Prescr. 2005;28(2).
Ranjan KP, Ranjan N, Bansal SK, Arora D. Prevalence of Pseudomonas aeruginosa in post-operative wound infection in a referral hospital in Haryana, India. J Lab Phys. 2011;2(2):129–32.
Li B, Webster TJ. Bacteria antibiotic resistance: new challenges and opportunities for implant-associated orthopedic infections. J Orthop Res. 2018;36(1):22–32.
Fadeyi A, Adigun I, Rahman G. Bacteriological pattern of wound swab isolates in patients with chronic leg ulcer. Int J Health Res. 2008. https://0-doi-org.brum.beds.ac.uk/10.4314/ijhr.v1i4.55375.
Iskandar K, Sartelli M, Tabbal M, Ansaloni L, Baiocchi GL, Catena F, et al. Highlighting the gaps in quantifying the economic burden of surgical site infections associated with antimicrobial-resistant bacteria. World J Emerg Surg. 2019;14(1):50.
Abayneh M, Asnake M, Muleta D, Simieneh A. Assessment of bacterial profiles and antimicrobial susceptibility pattern of isolates among patients diagnosed with surgical site infections at Mizan-Tepi University Teaching Hospital, Southwest Ethiopia: a prospective observational cohort study. Infect Drug Resist. 2022;15:1807–19.
Bitew Kifilie A, Dagnew M, Tegenie B, Yeshitela B, Howe R, Abate E. Bacterial profile, antibacterial resistance pattern, and associated factors from women attending postnatal health service at University of Gondar Teaching Hospital, Northwest Ethiopia. Int J Microbiol. 2018;2018:3165391.
Birhanu Y, Endalamaw A. Surgical site infection and pathogens in Ethiopia: a systematic review and meta-analysis. Patient Saf Surg. 2020;14:7.
Mengesha RE, Kasa BG, Saravanan M, Berhe DF, Wasihun AG. Aerobic bacteria in post surgical wound infections and pattern of their antimicrobial susceptibility in Ayder Teaching and Referral Hospital, Mekelle, Ethiopia. BMC Res Notes. 2014;7:575.
Garner JS. Hospital Infection Control Practice Advisory Committee. Guideline for isolation precaution in hospitals. Infection control and hospital epidemiology. Infect Control Hosp Epidemiol. 1996;17:53–80.
Cheesbrough M. District laboratory practice in tropical countries part II. 2nd ed. New York: Cambridge University Press; 2006. p. 45–58.
Clinical Laboratory Standard Institute. Performance standards for antimicrobial susceptibility testing; 30th ed. CLSI document M100. CLSI. 2021;M100.
Awoke N, Arba A, Girma A. Magnitude of surgical site infection and its associated factors among patients who underwent a surgical procedure at Wolaita Sodo University Teaching and Referral Hospital, South Ethiopia. PLoS ONE. 2019;14(12): e0226140.
Narula H, Chikara G, Gupta P. A prospective study on bacteriological profile and antibiogram of postoperative wound infections in a tertiary care hospital in Western Rajasthan. J Fam Med Prim Care. 2020;9(4):1927–34.
Ayala D, Tolossa T, Markos J, Yilma MT. Magnitude and factors associated with surgical site infection among mothers underwent cesarean delivery in Nekemte town public hospitals, western Ethiopia. PLoS ONE. 2021;16(4): e0250736.
Lubega A, Joel B, Justina LN. Incidence and etiology of surgical site infections among emergency postoperative patients in Mbarara regional referral hospital, South Western Uganda. Surg Res Pract. 2017. https://0-doi-org.brum.beds.ac.uk/10.1155/2017/6365172.
Shiferaw WS, Aynalem YA, Akalu TY, Petrucka PM. Surgical site infection and its associated factors in Ethiopia: a systematic review and meta-analysis. BMC Surg. 2020;20(1):1–15.
Badia JM, Casey AL, Petrosillo N, Hudson PM, Mitchell SA, Crosby C. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect. 2017;96(1):1–15.
Misha G, Chelkeba L, Melaku T. Incidence, risk factors and outcomes of surgical site infections among patients admitted to Jimma Medical Center, South West Ethiopia: prospective cohort study. Ann Med Surg (Lond). 2021;65: 102247.
Costa T, Medeiros P, Salles M. Smoking increases the risk of surgical site infection after hydrocelectomy in adults: a retrospective cohort study in Brazil. J Infect Dev Ctries. 2018;11:950.
Jiang C, Chen Q, Xie M. Smoking increases the risk of infectious diseases: a narrative review. Tob Induc Dis. 2020;18:60.
Vasundhara Devi P, Sreenivasulu Reddy P, Shabnum M. Microbial profile and antibiotic susceptibility pattern of orthopedic infections in a tertiary care hospital: a study from South India. Int J Med Sci Public Health. 2017;6(5):838–41.
Asres GS, Legese MH, Woldearegay GM. Prevalence of multidrug resistant bacteria in postoperative wound infections at Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia. Arch Med. 2017;9 (4):0.
Asres GS, Legese MH, Woldearegay GM. Prevalence of multidrug resistant Bacteria in postoperative wound infections at Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia. Archives of Medicine. 2017;9(4).
Mohammed A, Adeshina GO, Ibrahim YK. Incidence and antibiotic susceptibility pattern of bacterial isolates from wound infections in a tertiary hospital in Nigeria. Trop J Pharm Res. 2013;12(4):617–21.
Khanam RA, Islam MR, Sharif A, Parveen R, Sharmin I, Yusuf MA. Bacteriological profiles of pus with antimicrobial sensitivity pattern at a teaching hospital in Dhaka City. Bangladesh J. 2018. https://0-doi-org.brum.beds.ac.uk/10.3329/bjid.v5i1.37710.
Dessie W, Mulugeta G, Fentaw S, Mihret A, Hassen M, Abebe E. Pattern of bacterial pathogens and their susceptibility isolated from surgical site infections at selected referral hospitals, Addis Ababa, Ethiopia. Int J Microbiol. 2016. https://0-doi-org.brum.beds.ac.uk/10.1155/2016/2418902.
Bitew Kifilie A, Dagnew M, Tegenie B, Yeshitela B, Howe R, Abate E. Bacterial profile, antibacterial resistance pattern, and associated factors from women attending postnatal health service at University of Gondar Teaching Hospital, Northwest Ethiopia. Int J Microbiol. 2018. https://0-doi-org.brum.beds.ac.uk/10.1155/2018/3165391.
Kalayu AA, Diriba K, Girma C, Abdella E. Incidence and bacterial etiologies of surgical site infections in a Public Hospital, Addis Ababa, Ethiopia. Open Microbiol J. 2019. https://0-doi-org.brum.beds.ac.uk/10.2174/1874285801913010301.
Szaniawski MA, Spivak AM. Recurrent Paenibacillus infection. Oxf Med Case Rep. 2019;2019(5):omz034.
Tena D, Fernández C, Lago MR. Alcaligenes faecalis: an unusual cause of skin and soft tissue infection. Jpn J Infect Dis. 2015;68(2):128–30.
Patterson SB, Mende K, Li P, Lu D, Carson ML, Murray CK, et al. Stenotrophomonas maltophilia infections: clinical characteristics in a military trauma population. Diagn Microbiol Infect Dis. 2020;96(2): 114953.
de With K, Allerberger F, Amann S, Apfalter P, Brodt HR, Eckmanns T, et al. Strategies to enhance rational use of antibiotics in hospital: a guideline by the German Society for Infectious Diseases. Infection. 2016;44(3):395–439.
Ali KM, Al-Jaff BM. Source and antibiotic susceptibility of Gram-negative bacteria causing superficial incisional surgical site infections. Int J Surg Open. 2021;30:100318.
Mora-Guzmán I, Rubio-Perez I, Maqueda González R, Domingo Garcia D, Martín-Pérez E. Surgical site infection by carbapenemase-producing Enterobacteriaceae. A challenge for today's surgeons. Cir Esp (Engl Ed). 2020;98(6):342–9.
Ma F, Xu S, Tang Z, Li Z, Zhang L. Use of antimicrobials in food animals and impact of transmission of antimicrobial resistance on humans. Biosaf Health. 2021;3(1):32–8.
Acknowledgements
The authors would like to thank Addis Ababa University, Armauer Hansen Research Institute, Debre Tabor University, Uppsala University, and The Centre for Innovative Drug Development and Therapeutic Trials for Africa (CDT-Africa) for supporting this study. We would like to extend our gratitude to the Debre Tabor compressive specialized hospital, Tikur Anbessa Specialized Hospital, Hawassa University Teaching Hospital, and Jimma University Teaching Specialized Hospital for allowing us to conduct the study. We are thankful to the physicians, nurses, and microbiologists from all the study sites who helped us undertake this study. Lastly, our gratitude goes to all the study participants.
Funding
This study was sponsored by Addis Ababa University, Armauer Hansen Research Institute, Uppsala University, SIDA/SAREC bilateral research cooperation with Ethiopia and The Centre for Innovative Drug Development and Therapeutic Trials for Africa.
Author information
Authors and Affiliations
Contributions
SW: was the primary researcher, conceived the study, data collection, analysis, interpretation of the findings, drafting the manuscript, and write-up. AAl substantially participated in laboratory work. TA, BS, GS, AAb, AM and GTB: substantially participated in the design of the study, reviewed the manuscript, and provided critical intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance and approval were obtained from Addis Ababa University's College of Health Sciences and AAREC, AAUMF03-008/2020. Above all the data were collected after full informed and written consent or assent was obtained from each participant.
Consent for publication
Not applicable.
Competing interests
We authors declare that no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Worku, S., Abebe, T., Alemu, A. et al. Bacterial profile of surgical site infection and antimicrobial resistance patterns in Ethiopia: a multicentre prospective cross-sectional study. Ann Clin Microbiol Antimicrob 22, 96 (2023). https://0-doi-org.brum.beds.ac.uk/10.1186/s12941-023-00643-6
Received:
Accepted:
Published:
DOI: https://0-doi-org.brum.beds.ac.uk/10.1186/s12941-023-00643-6